Scleroderma
Scleroderma is an autoimmune disease that can affect your child’s skin and the connective tissues that protect their organs and other parts of their body. This chronic disease happens when your body makes too much collagen, a protein found all over your body in your hair, skin, nails, bones, ligaments and tendons.
This condition can range from mild skin changes to more serious issues affecting your child's internal organs. Our dedicated team of experts will work closely with you and your child's pediatrician to help you manage this condition and help improve your child's quality of life.
What is scleroderma?
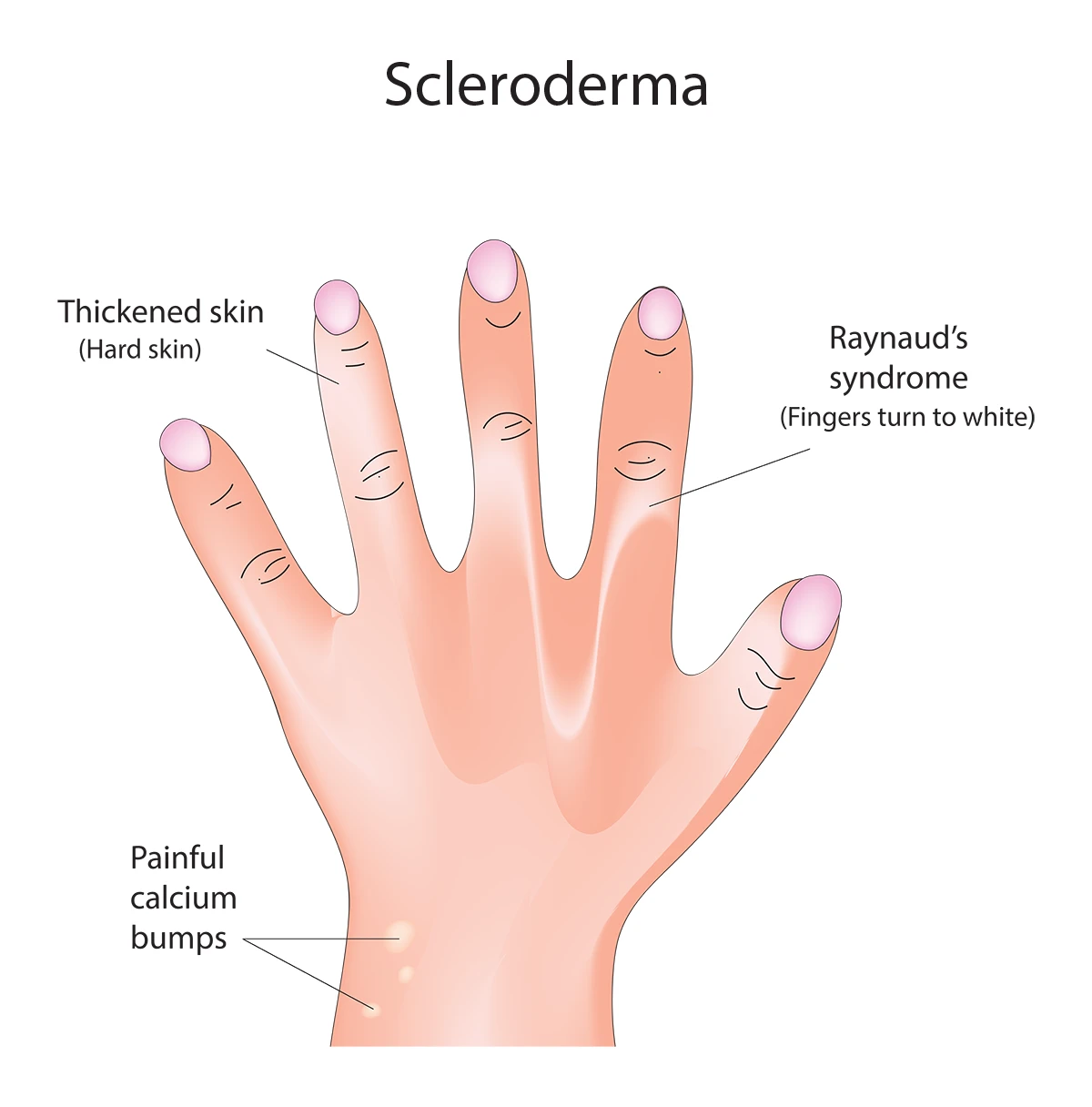
Common scleroderma symptoms include thickened skin, Raynaud’s syndrome and painful calcium bumps.
Scleroderma is a rare autoimmune skin disorder that typically affects people between the ages of 30 and 50. Scleroderma can affect children, although it is rare. When it occurs in children, it’s often called juvenile scleroderma.
This disease occurs when the immune system mistakenly attacks healthy tissue, leading to the production of too much collagen. This excess collagen causes the skin to become thick and hard.
The management of juvenile scleroderma typically involves a multidisciplinary approach, including pediatric rheumatologists, dermatologists, pulmonologists and other specialists, to address the specific symptoms and complications that arise.
What do scleroderma lesions look like?
Scleroderma lesions vary based on the type and severity:
- Localized lesions (morphea): Patches of thickened, shiny or smooth skin, often with a reddish or purplish border. Over time, they may become lighter or darker than the surrounding skin.
- Linear scleroderma: Narrow bands of hardened skin, often affecting limbs and potentially restricting movement.
- Systemic sclerosis skin changes: Tight, shiny skin over larger areas, particularly on the face, hands, or arms.
Types of scleroderma
Scleroderma can occur in two ways: localized and systemic. Each type of scleroderma has different symptoms and affects various parts of the body.
Localized scleroderma
Also known as morphea scleroderma, this type primarily affects the skin. It appears as shiny, thickened patches that may be uncomfortable or cosmetically concerning. Localized scleroderma doesn’t usually affect internal organs but can cause tightness and reduced movement in the affected areas.
Systemic scleroderma
Also called systemic sclerosis, this more severe type affects the skin, blood vessels and internal organs. There are two subtypes of systemic scleroderma:
- Limited cutaneous systemic sclerosis: This subtype can lead to complications such as pulmonary hypertension, where the heart struggles to pump blood into the lungs.
- Diffuse cutaneous systemic sclerosis: This subtype affects larger areas of skin and internal organs, potentially causing significant tissue damage and complications such as kidney failure or heart issues.
Scleroderma symptoms
Symptoms of scleroderma depend on the type and severity but may include:
- Hard, thickened skin: Often shiny and tight, especially on the hands, face, or extremities.
- Raynaud's syndrome: Reduced blood flow to fingers and toes, causing color changes and sensitivity to cold.
- Joint pain and stiffness: Stiff joints, particularly in the arms and legs, can limit mobility.
- Digestive problems: Acid reflux, difficulty swallowing, or poor nutrient absorption.
- Respiratory issues: Shortness of breath or reduced lung function.
- Facial changes: Tightened skin may make smiling or opening the mouth difficult.
What are the early stages of scleroderma?
The early stages of scleroderma can be subtle, making early diagnosis important to ensure your child gets proper treatment. Common early signs include:
- Raynaud's syndrome: This is often the first symptom people notice. It can occur years before other signs appear.
- Swelling of fingers and hands: Your child’s fingers and hands may feel puffy and swollen, especially in the morning.
- Skin changes: You may notice patches of thickened skin, which could be a sign of localized scleroderma.
- Fatigue and general discomfort: Feeling unusually tired or experiencing unexplained aches and pains can also be early indicators of scleroderma.
If you notice any of these symptoms in your child, schedule an appointment with their pediatrician or family doctor. They can rule out other conditions and refer you to a child rheumatologist if needed.
Complications of scleroderma
Without proper treatment, scleroderma can lead to serious complications, including:
- Pulmonary fibrosis: Scarring in the lungs, leading to breathing difficulties.
- Kidney problems: High blood pressure or kidney failure, known as scleroderma renal crisis.
- Heart issues: Scarring of heart tissue may cause irregular heartbeats or heart failure.
- Digestive damage: Scarring in the esophagus or intestines, leading to significant discomfort and nutrient deficiencies.
Scleroderma diagnosis
Diagnosing scleroderma involves a combination of physical exams, lab tests and imaging tests. Your child's doctor will review their medical history, discuss scleroderma symptoms and look for any changes in their skin, such as hard skin and Raynaud’s syndrome.
If you are referred to a child rheumatologist, they may order blood tests to check for specific antibodies associated with scleroderma. They may also do a skin biopsy where they take a small sample of your child's skin to look for excess amounts of collagen or tissue damage.
X-rays, CT scans or MRIs may be used to assess the extent of organ involvement and rule out other conditions.
Scleroderma treatment
There’s no cure for scleroderma, but several treatments can help manage symptoms and slow the progression of the disease. Your child’s rheumatologist will develop a scleroderma treatment plan that fits their specific needs based on the type of scleroderma and how severe it is.
Common scleroderma treatment options
- Medications: Drugs that suppress the immune system can help reduce inflammation and slow the disease’s progression. Other medications may be used to manage specific symptoms. These medications may include calcium-channel blockers for Raynaud’s syndrome or proton-pump inhibitors for acid reflux.
- Physical therapy: Regular physical therapy can help maintain your child’s joint flexibility and reduce stiffness.
- Skin care: Keeping your child’s skin moisturized and protected from the cold can help manage skin symptoms.
- Surgical options: In severe cases, surgery may be necessary to manage complications like severe Raynaud’s syndrome or blockages in your child’s digestive tract.
Can scleroderma go away?
Scleroderma is a chronic, long-lasting condition that doesn’t go away. Living with scleroderma can be challenging, but understanding the disease and working closely with your child’s care team can help navigate scleroderma’s complexities. Early diagnosis and a comprehensive treatment plan are key to managing scleroderma effectively.
Get care
Kid-focused. Close to home. We're here for your child in person and online.





