Bronchiectasis
Find a doctorAnytime your child is unable to breathe is a cause for concern. Advocate Children’s Hospital is here to help you ease your concerns and work with you and your family to manage any condition affecting your child’s ability to breathe.
Bronchiectasis is a long-term lung condition that involves permanent damage to the airways, making it harder for your child’s lungs to clear mucus. This condition can cause frequent lung infections, chronic coughing and the uncomfortable experience of coughing up mucus or phlegm.
While there’s no cure for bronchiectasis, it is very treatable. Our team of expert pulmonologists are with you every step of the way. They can help you manage your child’s symptoms so they can get back to being a kid.
What is bronchiectasis?
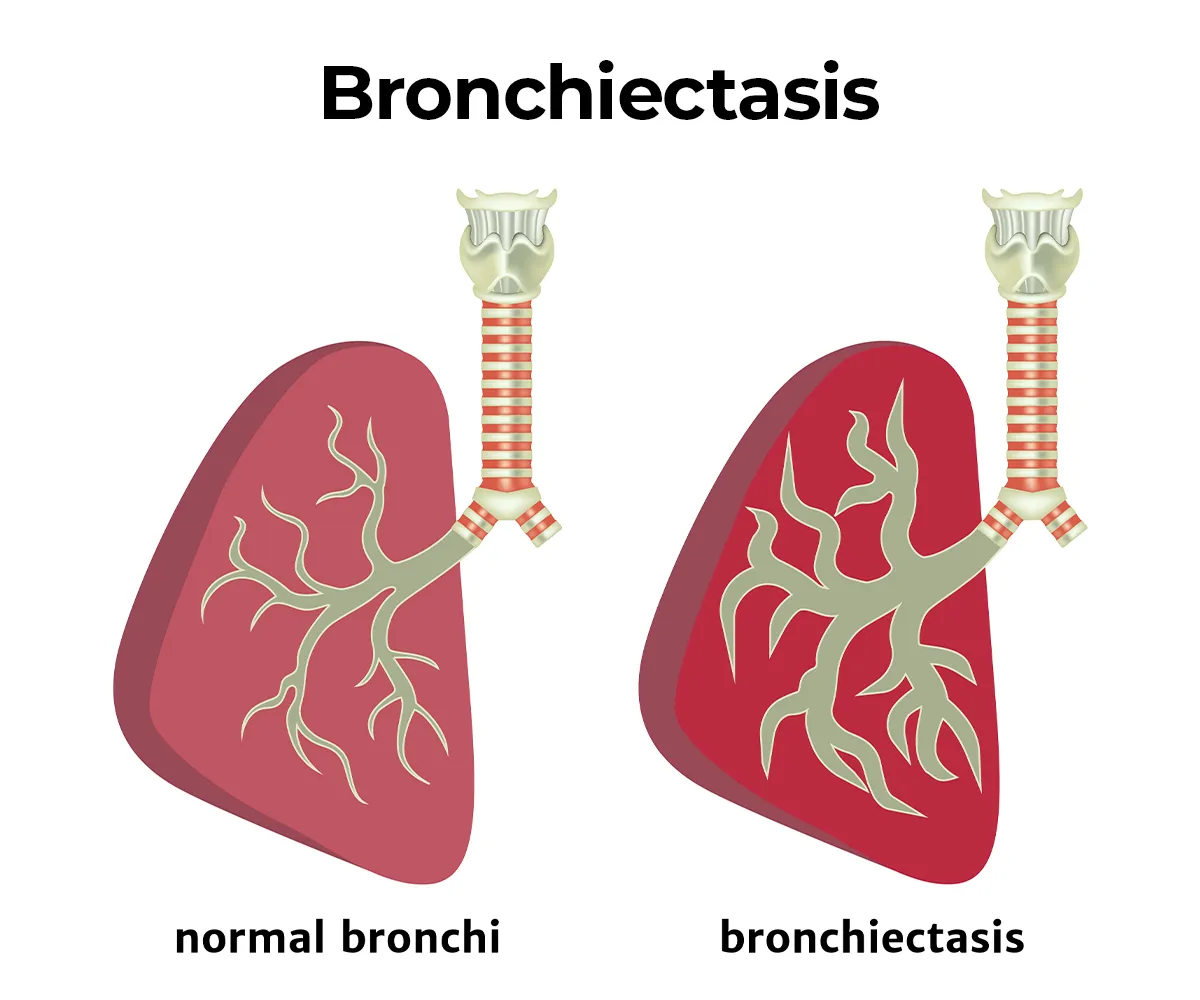
The illustration compares a normal lung to a lung affected by bronchiectasis with wing airway dilation and damaged bronchi.
Bronchiectasis is a condition where the airways in the lungs, called bronchi, become permanently widened due to inflammation and infection. These airways lose their ability to clear mucus effectively, allowing bacteria to grow and causing recurrent respiratory infections.
The result is a cycle of lung damage, infections and inflammation, making it harder to breathe and leading to chronic coughing.
Most cases of bronchiectasis are caused by cystic fibrosis. However, in some instances, non-cystic fibrosis bronchiectasis (non-CF bronchiectasis) refers to cases of bronchiectasis not caused by cystic fibrosis. This distinction is important because the underlying causes and treatments can vary between the two conditions.
What’s the difference between bronchiectasis and bronchitis?
Bronchiectasis and bronchitis are both lung conditions that involve inflammation of the airways, but they’re not the same.
Bronchiectasis is a long-term condition where the airways become permanently damaged and widened. It leads to chronic symptoms like coughing up mucus, recurrent infections and lung damage.
Bronchitis can be either acute or chronic, often triggered by infections or irritants like allergens. Acute bronchitis usually resolves within a few weeks, while chronic bronchitis is a long-term condition but doesn’t cause permanent airway damage the way bronchiectasis does.
What are the types of bronchiectasis?
There are three types of bronchiectasis, which are classified based on the shape and structure of the damaged airways. Each type affects the lungs differently. They include:
- Cylindrical bronchiectasis: The airways are uniformly widened.
- Varicose bronchiectasis: The airways have irregular shapes, with areas of widening and narrowing.
- Cystic bronchiectasis: The airways develop large, balloon-like cysts. This is the most severe type.
What is the most common type of bronchiectasis?
Cylindrical bronchiectasis is the most common type. It involves a uniform widening of the airways, which leads to chronic coughing and mucus buildup. While it’s less severe than other forms, it still requires ongoing care and treatment to manage the symptoms.
What are the stages of bronchiectasis?
Bronchiectasis progresses in stages, starting with mild symptoms that can become more severe over time. Early recognition is key to slowing the progression:
- Mild: Occasional coughing with mucus, usually following respiratory infections.
- Moderate: Persistent coughing with mucus, wheezing and difficulty breathing. Lung infections may become more frequent.
- Severe: Frequent infections, chronic coughing up mucus or blood and worsening shortness of breath.
Bronchiectasis symptoms
If your child has bronchiectasis, they may experience a range of symptoms that can impact their daily lives. Some of the most common symptoms include:
- Chronic coughing
- Coughing up mucus
- Shortness of breath
- Frequent lung infections
- Coughing up blood
- Wheezing
Bronchiectasis diagnosis
Diagnosing bronchiectasis requires a combination of medical history, physical examination and imaging tests, such as X-rays or a bronchiectasis CT scan, which provides detailed images of the lungs and airways. This test helps doctors assess the extent of lung damage and identify the specific type of bronchiectasis so they can provide your child with the right treatment.
Your doctor may also check for bacteria in the mucus by testing a sample. They may also do a lung function test to see how well your child’s lungs are working.
Treatment for bronchiectasis
While there is no cure for bronchiectasis, treatment focuses on managing symptoms, preventing infections and improving lung function. The goal is to reduce the risk of further lung damage and help your child maintain a healthy, active lifestyle.
Your child’s care team may include a pediatric rheumatologist to develop a treatment plan to better meet your child’s specific needs. Common bronchiectasis treatments include:
- Airway clearance therapy: Techniques such as chest physiotherapy and breathing exercises help loosen mucus from the lungs, making it easier to cough up.
- Bronchiectasis medications: Antibiotics are often prescribed to treat or prevent lung infections. Inhalers or bronchodilators may also be used to open the airways and reduce shortness of breath.
- Bronchiectasis therapies: Regular physical activity and pulmonary rehabilitation programs, such as physical therapy, can strengthen the lungs and improve your child’s breathing.
- Surgery: In rare cases, your doctor may recommend surgery if the damage is localized to one area of the lung.
Your child’s care team will develop a personalized treatment plan based on their symptoms and overall health, which may include a combination of these therapies and ongoing monitoring.
Get care
Kid-focused. Close to home. We're here for your child in person and online.





