Allergic bronchopulmonary aspergillosis (ABPA)
Find a doctorIt can be scary to see your child have trouble breathing, especially when it happens suddenly, and you don’t know why. It could be due to seasonal allergies or asthma. However, it could be a reaction to a common mold known as aspergillus that may be found in your home or outside.
Our team of allergy and asthma specialists is here to help you find the answers you need. They will work with your pediatrician to develop a treatment plan for your child so they can get back to being a kid.
What is allergic bronchopulmonary aspergillosis?
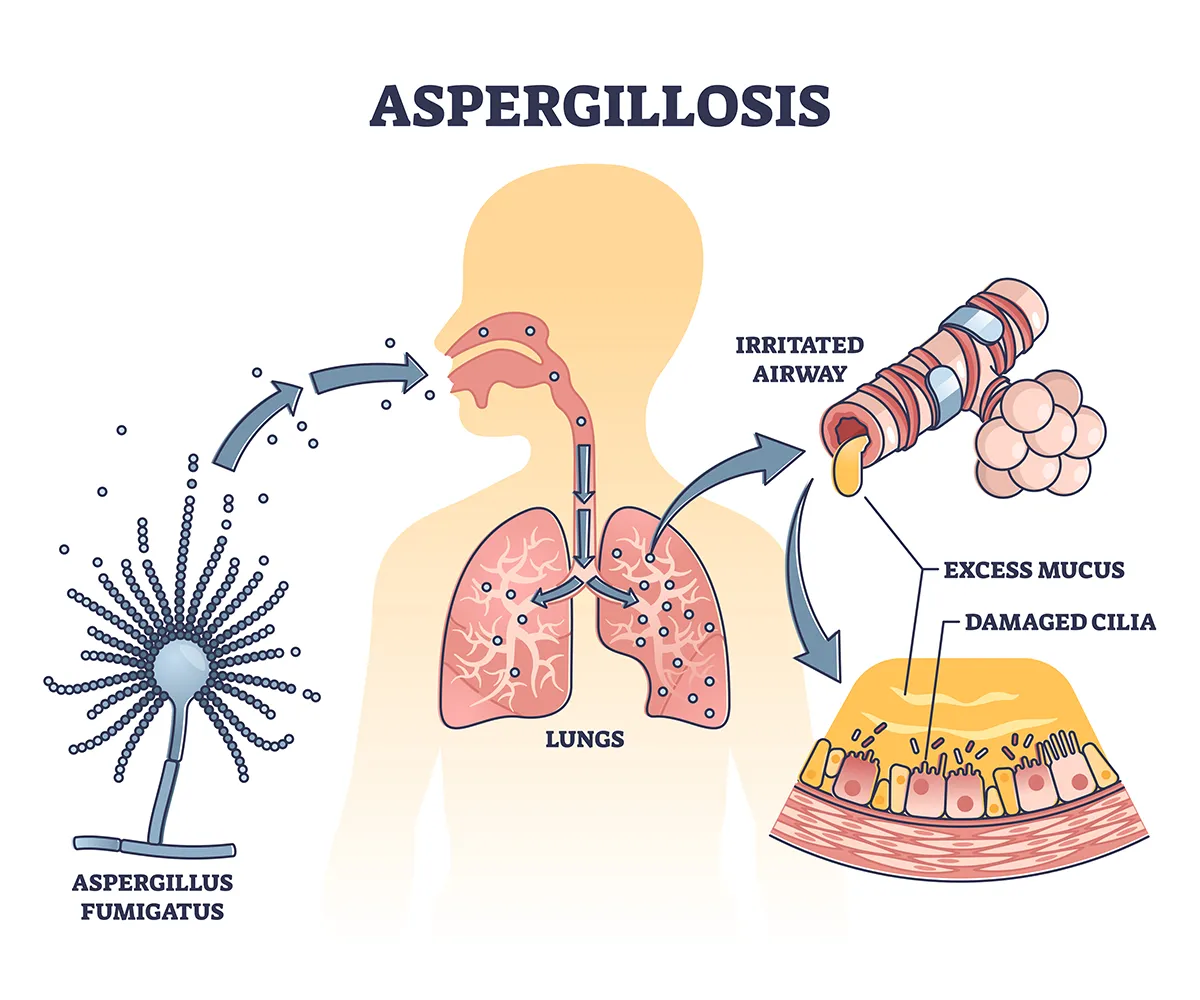
Aspergillus fumigatus spores are inhaled and enter the lungs, causing airway irritation, excess mucus and damage to cilia.
Allergic bronchopulmonary aspergillosis (ABPA) is a reaction to Aspergillus mold, primarily aspergillus fumigatus. Aspergillus mold is often found in soil, dead leaves and plants, some foods and damp indoor environments.
When the mold spores are inhaled, they cause a severe allergic response, particularly if your child has allergies or preexisting lung conditions such as asthma or cystic fibrosis. This response leads to inflammation of the airways and the formation of mucus plugs and can cause damage to the air sacs in the lungs, making it difficult to breathe.
What causes allergic bronchopulmonary aspergillosis?
While most children can inhale Aspergillus spores without any issues, children with asthma, cystic fibrosis or weakened immune systems may experience a severe allergic reaction when exposed to the mold.
When Aspergillus spores are inhaled, they can become trapped in the airways. This alerts your immune system which mistakes the mold spores as a threat and causes inflammation and mucus production. Over time, this immune response can lead to chronic lung damage, scarring and the potential for fungal pneumonia, resulting in the characteristic symptoms of allergic bronchopulmonary aspergillosis.
What causes allergic bronchopulmonary aspergillosis?
While most children can inhale Aspergillus spores without any issues, children with asthma, cystic fibrosis or weakened immune systems may experience a severe allergic reaction when exposed to the mold.
When Aspergillus spores are inhaled, they can become trapped in the airways. This alerts your immune system which mistakes the mold spores as a threat and causes inflammation and mucus production. Over time, this immune response can lead to chronic lung damage, scarring and the potential for fungal pneumonia, resulting in the characteristic symptoms of allergic bronchopulmonary aspergillosis.
How common is allergic bronchopulmonary aspergillosis?
ABPA is considered a rare condition, but it's more common if your child has asthma or cystic fibrosis. If your child has one of these underlying conditions, it is important to be aware of the potential for allergic bronchopulmonary aspergillosis, especially if their symptoms worsen or become more difficult to control with normal treatments.
What are the symptoms of allergic bronchopulmonary aspergillosis?
It can be hard to notice APBA symptoms in your child because they often resemble those of other respiratory conditions. This can make diagnosing allergic bronchopulmonary aspergillosis challenging for your child’s pediatrician or allergist.
Common aspergillosis symptoms include:
- Chest tightness and discomfort
- Coughing up blood in severe cases
- Fatigue and general discomfort
- Persistent cough that may produce mucus or mucus plugs, thick jelly-like strings of mucus
- Recurrent episodes of bronchitis or pneumonia
- Wheezing and shortness of breath
Diagnosing allergic bronchopulmonary aspergillosis
Diagnosing ABPA can be challenging due to its overlap with other respiratory conditions. However, early diagnosis is vital to prevent long-term lung damage and to manage the condition effectively.
Your doctor will ask about your child’s possible exposure to Aspergillus mold and do a physical exam. They may take a sample of mucus to check for aspergillus spores or other signs of fungal infection.
Tests for allergic bronchopulmonary aspergillosis
To rule out other allergies or an allergic reaction to Aspergillus, your doctor may refer your child to an allergist for allergy testing. This is done through a skin-prick test. An allergist or nurse will put a tiny amount of liquid that contains the Aspergillus mold into the skin through a small scratch or prick on the skin. They’ll wait for about 15 minutes to check for a red, raised bump on the skin.
Blood tests also may be used to measure levels of specific antibodies such as immunoglobulin E (IgE), which is often elevated in allergic reactions and conditions.
Chest X-rays or CT scans can reveal characteristic changes in the lungs, such as bronchiectasis, a chronic lung condition where the airways are widened, or mucus plugging.
Allergic bronchopulmonary aspergillosis treatments
There are several ways to treat and manage APBA. Your child’s care team will work with you to create a treatment plan to address your child’s allergy and fungal infection.
Your child may find relief by avoiding places the Aspergillus mold is commonly found. Other aspergillosis treatment options include:
- Corticosteroids: These medications, such as prednisone, help reduce airway inflammation and prevent the immune system from overreacting to the Aspergillus spores.
- Antifungal medications: Drugs like itraconazole or voriconazole may be prescribed to reduce fungus in the lungs and prevent the growth of Aspergillus. These are often used in cases where corticosteroids are not sufficient by themselves.
- Bronchodilators: Inhaled medications that help open the airways can be useful in managing asthma-like symptoms associated with ABPA.
If your child has ABPA they should have regular appointments with their pediatrician or allergist to monitor lung function, adjust medications and detect any signs of worsening lung disease.
Can allergic bronchopulmonary aspergillosis be cured?
There is no cure for ABPA, but with appropriate management, the condition can be controlled. The goal of treatment is to reduce inflammation, manage allergic responses and prevent further lung damage. Early diagnosis and ongoing care are important for proper management and preventing complications.
What happens if allergic bronchopulmonary aspergillosis goes untreated?
If left untreated, ABPA can lead to serious complications, including chronic fungal lung infections, irreversible lung damage and respiratory failure.
Over time, repeated inflammation and scarring can cause the airways to become permanently damaged, resulting in bronchiectasis. This can make it even more difficult for your child to clear mucus from their lungs, leading to recurrent infections and further deterioration of lung function.
Get care
Kid-focused. Close to home. We're here for your child in person and online.





