Atopic dermatitis (eczema)
Atopic dermatitis, commonly referred to as eczema, is a common skin condition in children. Characterized by dry, itchy skin and patches of redness, atopic dermatitis can cause discomfort and frustration for children and parents alike.
Eczema affects people of all ages, but it often begins in infancy, with many experiencing “baby eczema.” Though the exact cause of atopic dermatitis is unclear, it’s often linked to factors like genetics, environmental causes and allergies.
If your child is dealing with eczema, Advocate Children’s Hospital is here to help with compassionate care, advanced treatment options and support to help your child find relief.
What is atopic dermatitis?
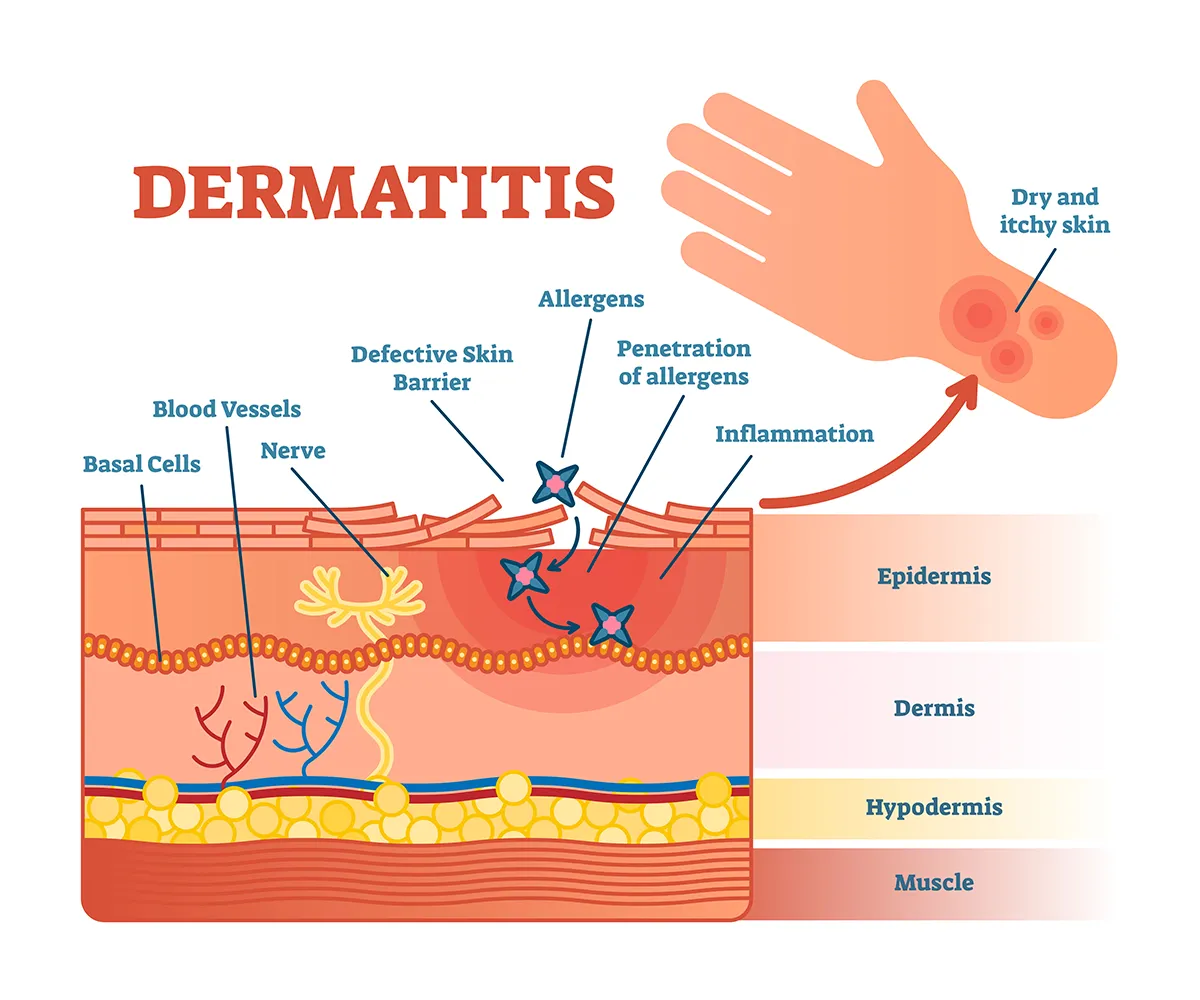
Atopic dermatitis, or eczema, is a chronic condition that causes the skin to become dry, itchy and irritated. This disease often appears as patches of red, inflamed skin that can crack and, in some cases, swell or ooze.
Atopic dermatitis is just one type of dermatitis, which refers to skin inflammation in general, but it’s the most common form found in children. Often linked to food allergies or asthma, eczema can also be caused by environmental factors like dry weather or certain fabrics.
What does atopic dermatitis look like?
Atopic dermatitis can appear differently depending on your child’s age and the severity of the symptoms. Commonly, it shows up as red, itchy patches on the face, scalp, arms or legs. In babies, it often appears on the cheeks, known as “eczema on face.” Older children might experience patches in the folds of their elbows, knees or neck.
The skin may look scaly, dry, or swollen and, when scratched, can become cracked or even infected. These eczema rashes can look different on each child and may range from small, red patches to widespread areas of thick, leathery skin.
Types of eczema
Eczema includes several types, each with unique causes and symptoms. Recognizing the specific type of eczema is helpful to ensure your child gets effective treatment:
- Atopic eczema: This is the most common form and is typically linked to allergies and a family history of asthma or hay fever.
- Contact dermatitis: This type occurs when the skin reacts to contact with an irritant or allergen, like certain soaps or metals.
- Seborrheic dermatitis: Often found on the scalp, this type appears as scaly patches and redness, commonly known as “scalp eczema.”
What are the causes of eczema?
The exact cause of eczema isn’t fully understood, but it’s thought to be influenced by genetic and environmental factors. Children with family histories of eczema, asthma or allergies are more likely to develop it. Common causes include:
- Allergens: Food allergies, pet dander, pollen and dust can trigger eczema symptoms.
- Environmental factors: Extreme temperatures, low humidity, and irritants like smoke or harsh soaps can worsen symptoms.
- Genetics: Children with a family history of eczema or other allergic conditions are at higher risk.
These causes may lead to an allergic skin reaction, leading to the dry, itchy skin associated with eczema.
Atopic dermatitis symptoms
Eczema symptoms can vary but often include:
- Itchy skin: Constant itchiness that’s often worse at night.
- Redness and swelling: Skin appears red, inflamed and sometimes swollen.
- Cracking and scaly patches: Skin may become rough, cracked and scaly, especially on affected areas like the elbows, knees, and face.
- Thickened skin: Frequent scratching can cause skin to thicken over time, leading to areas with a leathery texture.
Diagnosing eczema
Diagnosing eczema usually involves a physical exam and a review of your child’s medical history. Your pediatrician may also ask about your family history of allergies or asthma.
Sometimes, skin tests or blood tests are performed to identify allergens that may cause or worsen symptoms, especially if food allergies are suspected. Identifying these causes can help doctors create a targeted treatment plan.
Your pediatrician may work closely with a dermatologist or an allergist to provide comprehensive care to ensure your child is getting the treatment they need.
Eczema treatments
Treatment for eczema focuses on reducing symptoms and managing flare-ups. Some common treatments for eczema include:
- Moisturizers: Regularly applying a thick, unscented moisturizer helps to hydrate dry skin and create a protective barrier.
- Prescription creams: Anti-inflammatory creams can reduce redness, swelling and itching.
- Topical steroids: Low-dose steroid creams may be prescribed to manage inflammation during flare-ups.
- Antihistamines: These can reduce itching and are especially helpful at night to prevent scratching.
- Lifestyle adjustments: Using gentle, fragrance-free soaps and laundry detergents, wearing soft fabrics and keeping the skin covered in extreme weather can help prevent irritation.
Your doctor will discuss the best atopic dermatitis treatments for your child’s unique needs, including both topical treatments and preventive measures to reduce flare-ups.
Complications of atopic dermatitis
While eczema is manageable, it can lead to complications if not treated properly. Potential complications include:
- Skin infections: Constant scratching can lead to cracked skin, which may become infected by bacteria or viruses.
- Sleep disturbances: The persistent itchiness can make it difficult for children to get a good night’s sleep, affecting their overall health.
- Emotional impact: Eczema can be challenging for your child and impact their self-esteem, especially if the eczema is visible on the face or hands.
How to prevent eczema
While eczema can’t be entirely prevented, certain measures can help reduce the frequency and severity of flare-ups:
- Avoid known causes: Identifying and avoiding known causes, such as certain foods, harsh soaps or pet dander, can reduce symptoms.
- Maintain skin hydration: Regular moisturizing helps to keep skin hydrated, reducing dryness and itchiness.
- Dress in breathable fabrics: Choosing soft, cotton clothing over synthetic fabrics helps avoid irritation.
- Use gentle skincare products: Using fragrance-free, hypoallergenic products are less likely to irritate sensitive skin.
Get care
Kid-focused. Close to home. We’re here for your child in person and online.





